Choosing an Electronic Medical Record (EMR) system can feel like trying to navigate a new city without a map. There are countless options, each with its own layout and rules, and the best EMR system for your practice depends entirely on what you do, whether that's managing aesthetic workflows in a medspa or tracking chronic diseases in a primary care clinic.
This guide will be your map, cutting through the jargon to explain the core concepts you actually need to know.
Understanding the Landscape of Different EMR Systems
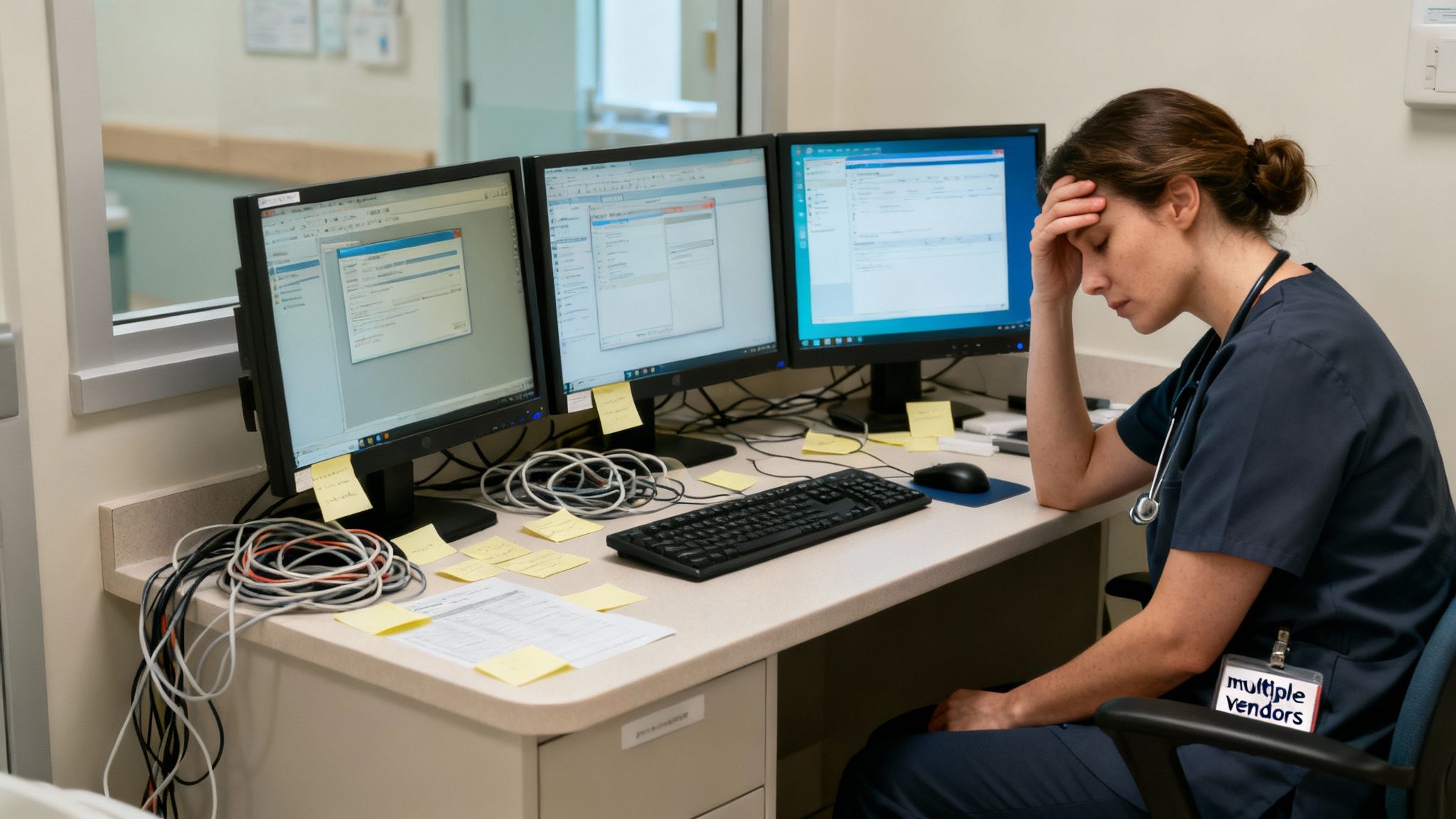
Most modern practices are drowning in software. It's not uncommon to be juggling 8 to 12 different vendors just to handle day-to-day tasks like billing, scheduling, and patient communication. This patchwork approach creates a nightmare of data silos, security risks, and just plain inefficiency. Your staff ends up bouncing between different logins and platforms, manually re-entering data and wasting precious time that should be spent with patients.
But the tide is turning. The global hospital EMR market, valued at a staggering USD 19.16 billion in 2024, is expected to soar to USD 29.97 billion by 2030. This isn't just growth; it's a clear signal that the industry is moving away from clunky, disconnected tools toward smarter, more integrated solutions. You can dig deeper into this market trend over at marknteladvisors.com.
Core Concepts You Need to Know
Before you can even begin comparing different EMRs, you have to get a handle on the foundational models they're built on. These concepts dictate everything from your upfront costs and maintenance headaches to how you access your data and how easily you can grow.
Think of it like this: are you buying a pre-built house or designing a custom one? The answer depends on two key distinctions:
- Deployment Model: Where does the software actually live? Is it running on a server tucked away in your office closet (on-premise), or do you access it over the internet from a secure, remote data center (cloud-based)?
- Architectural Design: How is the system put together? Is it one massive, all-in-one program with rigid features (monolithic), or is it a collection of specialized modules designed to work together seamlessly (integrated)?
The real goal here is to stop patching together a dozen different tools and find a single, unified platform. A vertically integrated system is built from the ground up to handle everything, ensuring every part of your practice—from charting to billing—is perfectly in sync.
Why Your Practice Type Matters
A one-size-fits-all EMR is a recipe for disaster. The daily grind of a busy primary care clinic is worlds away from the client-focused workflow of a boutique medspa or a concierge practice.
A system built for managing chronic illness probably won't have the tools you need to track cosmetic treatment packages or manage before-and-after photo galleries. This is why connecting your EMR choice to your overall business strategy is so important. If you want to learn more, our guide on what is practice management software is a great place to start.
Ultimately, picking the right system means finding one that matches what you do every single day, so the technology actually helps you work better, not harder.
On-Premise vs. Cloud-Based EMRs: Choosing Your Foundation
When you're picking an EMR system, the first big decision you'll make is where it will "live." This isn't just a technical detail; it's a foundational choice that shapes your budget, workflow, and day-to-day operations.
Think of it like deciding between buying a house (on-premise) and renting a fully-serviced luxury apartment (cloud-based). One gives you total control but comes with all the responsibilities of ownership, while the other offers convenience and predictability for a monthly fee. This is the first, and most critical, fork in the road.
What Is An On-Premise EMR?
The on-premise model is the old-school way of doing things. You purchase the servers, find a secure, climate-controlled space for them in your office, and either hire an IT team or keep a consultant on retainer to install, manage, and secure everything.
This approach gives you absolute control over your patient data and the entire system infrastructure. However, that control comes at a steep price. The upfront capital required for hardware, software licenses, and setup can be enormous, and that's before you even factor in the ongoing costs of maintenance, upgrades, and IT salaries.
What Is A Cloud-Based EMR?
In stark contrast, a cloud-based EMR runs on a subscription model, often called Software-as-a-Service (SaaS). With this setup, you don't own any hardware or software. Instead, you pay a predictable monthly or annual fee to a vendor who handles all the heavy lifting behind the scenes.
Your vendor takes care of everything from server maintenance and security patches to data backups and software updates, freeing you from the technical headaches.
The Financial Shift: From Capital Expense to Operating Expense
The most significant difference between these two models is how they impact your clinic's finances. On-premise solutions are a massive Capital Expense (CapEx)—a huge upfront investment that ties up a significant amount of cash.
Cloud-based systems, on the other hand, are a predictable Operating Expense (OpEx). This recurring cost is much easier to budget for. It also lets you direct your capital toward things that actually grow your practice, like marketing, new patient-facing equipment, or hiring top-tier staff. For modern medspas and specialty clinics that need to be nimble, this financial flexibility is a game-changer.
This is precisely why the market is shifting so dramatically. Cloud-based EMR deployments are on track to capture 80.1% of the global market share by 2025 as practices race to cut costs and improve their ability to scale. You can dig into the numbers yourself in this global EMR market report.
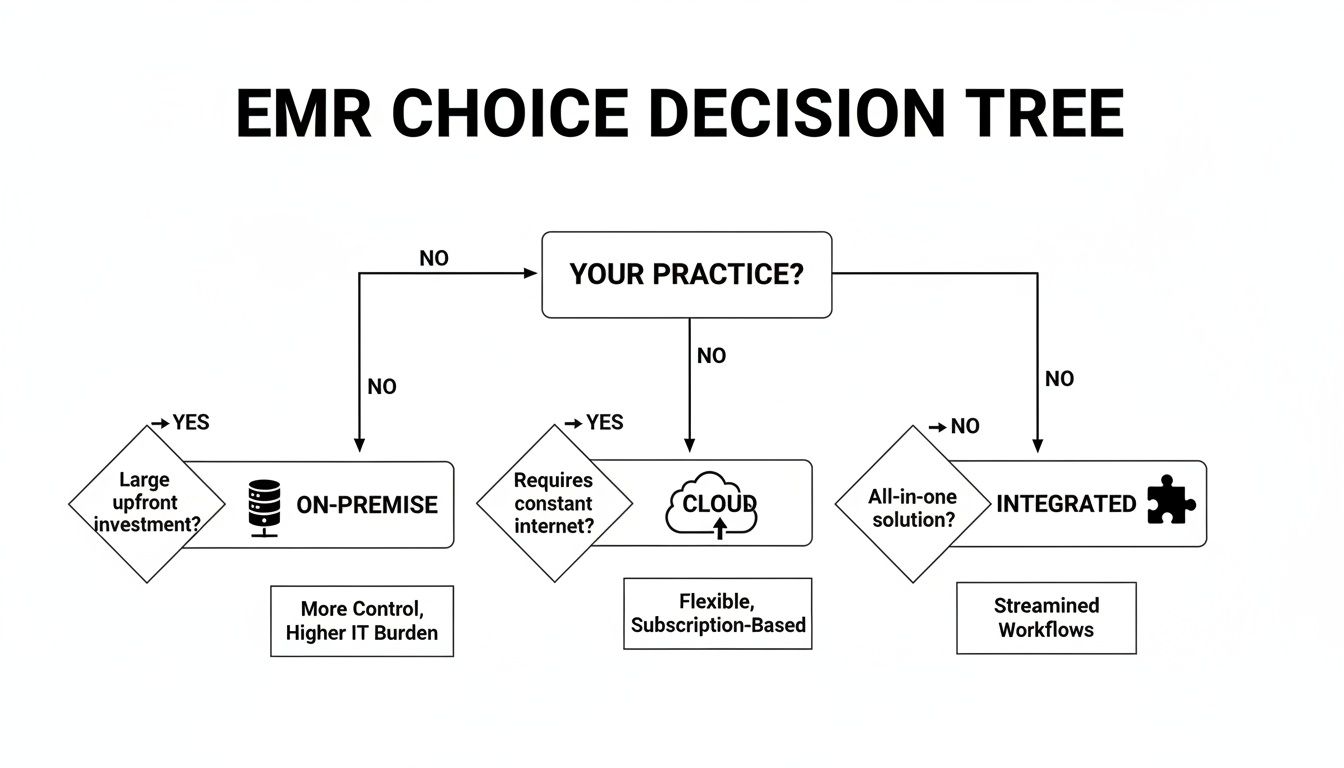
This decision tree gives you a quick visual guide to the core differences between deployment models.
As the graphic shows, cloud systems are built for the scalability and easy access that modern, growing practices demand.
To make the comparison even clearer, let's break it down side-by-side using our house vs. apartment analogy.
On-Premise vs Cloud-Based EMR: A Head-to-Head Comparison
| Factor | On-Premise EMR (The 'House') | Cloud-Based EMR (The 'Apartment') |
|---|---|---|
| Initial Cost | High CapEx: Requires major investment in servers, software licenses, and IT setup. | Low OpEx: Minimal upfront cost, with predictable monthly or annual subscription fees. |
| Maintenance | Your Responsibility: You handle all updates, security, backups, and hardware repairs. | Vendor's Responsibility: The provider manages all backend maintenance and updates automatically. |
| Accessibility | Limited: Access is typically restricted to your office's local network. Remote access is complex. | Anywhere Access: Log in from any device with an internet connection. Perfect for multiple locations. |
| Scalability | Difficult & Expensive: Adding new users or locations requires buying more hardware and licenses. | Effortless: Simply upgrade your subscription plan to add users or services as you grow. |
| Security | Your Burden: You are fully responsible for HIPAA compliance and protecting against cyber threats. | Shared Burden: Reputable vendors invest millions in security and compliance, taking on the heavy lifting. |
| Implementation | Long & Complex: Can take months to deploy, configure, and train staff on the new system. | Fast & Simple: Implementation is much quicker as no hardware installation is needed. |
For today's ambitious private practices, medspas, and specialty clinics, the agility, predictable costs, and reduced IT burden of a cloud-based EMR almost always make it the smarter choice. It lets you focus on what you do best—caring for patients—not on managing servers.
This modern approach fits perfectly with the operational efficiency you'll find in the best practice management software on the market today. By choosing a cloud foundation, you're setting your practice up for sustainable growth without the technical and financial headaches of an on-premise system.
Comparing Monolithic and Integrated EMR Platforms
Once you've figured out where your EMR will live (on-premise or in the cloud), the next big decision is how it's built. This is all about the system’s architecture, and it really boils down to two competing philosophies: monolithic versus integrated.
Getting this choice right is absolutely essential to avoid the operational headaches that bog down so many practices.
Think about one of those old-school flip phones from the early 2000s. It did its job—making calls, sending texts—but that was its entire world. You couldn't just download a new app or easily connect it to other gadgets. That’s a monolithic EMR in a nutshell: a single, self-contained system where every single feature is hardwired together.
The Limits of Monolithic Systems
A monolithic platform is often a straitjacket for a growing practice. Because everything is so tightly bundled, adding a new capability like a patient portal or telehealth isn't a simple upgrade; it can mean a massive, system-wide overhaul.
This closed-off design creates some serious, real-world problems:
- Data Silos: Information gets stuck inside the EMR. Trying to get that data to talk to your billing software, a pharmacy, or a lab often involves clumsy manual workarounds that are just begging for errors.
- Poor Scalability: As your practice expands, a monolithic system just can't keep pace. It wasn’t built to adapt to new services, more providers, or a bigger patient load.
- Vendor Lock-In: You’re completely at the mercy of one company for every update, fix, and feature request. It leaves you with zero flexibility and very little negotiating power.
You see these kinds of systems all the time in huge hospital networks, where giants like Epic Systems Corporation are king. While Epic's U.S. revenue is projected to hit $5.61 billion in 2025, their complex, one-size-fits-all structure is a notoriously bad fit for nimble private practices that need to adapt quickly. You can dig deeper into EHR industry statistics to see how different systems are carved out for specific markets.
The Power of Integrated Platforms
Now, picture a modern smartphone. Its real magic isn't the phone itself, but the ecosystem of specialized apps that all run on a single, shared operating system. This is exactly how an integrated EMR works. It uses a modular design where core functions are connected through APIs (Application Programming Interfaces), which act like universal translators between different software components.
This kind of architecture lets different "apps"—for scheduling, billing, clinical charting, and patient messaging—communicate with each other seamlessly. The flexibility is incredible. You can add, remove, or swap out tools as your practice’s needs change over time.
An integrated platform breaks down the walls between different parts of your practice. It ensures that when a patient's information is updated in one place—like their chart—it's instantly and accurately reflected everywhere else, from the front desk schedule to the billing department.
But there's a catch. Many systems that call themselves "integrated" are really just a collection of third-party tools bolted together. Each connection is a potential point of failure.
The gold standard is a truly vertically integrated platform, like Ragnar STACK, where every single component is developed by the same team to work together from day one. This eliminates the friction, security gaps, and hidden costs that come from juggling multiple vendors. What you get is a single, unified ecosystem that just works.
Finding an EMR Tailored to Your Medical Specialty
Trying to run a specialty clinic with a generic EMR is like asking a world-class chef to cook a five-star meal with just a butter knife. Sure, they might get the job done, but it’s going to be messy, inefficient, and a huge source of frustration.
The workflows that work perfectly well for a giant hospital network or a general family practice just don't map onto the day-to-day reality of a boutique medspa, a concierge clinic, or any other specialized practice. Picking a system that was actually built for your field isn’t just a nice-to-have; it's the foundation for giving great care and running a smart business.
Why Generic Systems Fail Specialized Practices
The simple truth is that different medical specialties operate in completely different worlds. A medspa's success hinges on visual charting, selling service packages, and offering a slick online booking experience. A concierge practice, on the other hand, needs robust tools to manage different membership levels and provide that high-touch, personalized service.
A generic, one-size-fits-all EMR can’t possibly excel in these different environments. Can you imagine an aesthetician trying to chart a Botox treatment using a template designed for tracking high blood pressure? It's more than just clunky—it’s clinically wrong. These systems are missing the specific forms, templates, and workflows you rely on every single day.
A busy medspa, for example, absolutely needs the ability to:
- Manage Treatment Packages: Easily track how many sessions of laser hair removal a client has used.
- Showcase Visual Progress: Keep a clean, high-resolution gallery of before-and-after photos that are simple to compare.
- Handle Retail Sales: Run a point-of-sale system for skincare products right within the patient's chart.
- Simplify Online Booking: Let clients book specific aesthetic services themselves without tying up the front desk.
None of these are standard-issue features in an EMR built for a primary care doctor, who is far more concerned with chronic disease management and preventive care reminders. Forcing a generic system to work for you inevitably leads to poor care and a burned-out team. In fact, a 2024 report found that 75% of users felt their modernized but poorly-matched system actually made them less efficient.
The right EMR shouldn’t force you to change how you work. It should feel like a natural extension of your practice, making your team faster, smarter, and more precise. A purpose-built system is designed with your specialty's best practices in mind from the very beginning.
The Strategic Advantage of a Specialty-Specific EMR
When you invest in an EMR built for your niche, you're doing more than just buying software. You're giving your practice a serious competitive edge. With technology that’s perfectly in sync with your clinical and business needs, everything starts to click.
A specialty-specific platform gives your providers the exact charting tools they need, improving clinical accuracy and saving time. It also automates all those little administrative tasks like appointment reminders, package tracking, or membership billing that can bog down your staff. This frees everyone up to focus on what really moves the needle: giving patients an incredible experience. If you're looking for more on this, our guide to finding the best EMR for private practice dives deep into how these tailored solutions can change the game.
Ultimately, you need a system that speaks your language. When your software gets what you do, every task is simpler, every workflow is smoother, and your practice is set up to provide better, more efficient care.
What Every Modern EMR Absolutely Needs
So, beyond just being a digital version of a paper chart, what makes a modern EMR truly work for a practice? When you start comparing the different EMR systems out there, you'll quickly realize that a few key features are no longer optional—they're essential for running an efficient, patient-focused practice. Think of this as your must-have list.
These aren't just bells and whistles. They're the gears that make a successful practice run smoothly. They cut down on the administrative grind, help you deliver better care, and honestly, just make life easier for your staff and your patients. If your system lacks these, you're working harder than you need to be.
Tools for Patient Engagement and Easy Access
Today's patients expect the same convenience from their doctor's office that they get from Amazon. That means a simple, intuitive patient portal isn't just a "nice-to-have"; it's a basic requirement. This is their secure spot to manage their healthcare, which takes a huge load off your front desk.
A good portal should let patients:
- Book Appointments Online: They can see open slots and book, reschedule, or cancel 24/7 without ever picking up the phone.
- Fill Out Digital Forms: Patients handle all the paperwork from their couch before they even walk in the door. This means no more clipboards and far fewer data entry errors.
- Message Your Team Securely: A HIPAA-compliant way for them to ask a quick question or request a refill without playing phone tag.
- See Their Own Health Info: Giving patients access to their lab results, visit notes, and treatment plans empowers them to take an active role in their care.
A great patient portal does more than just save time. It turns a patient into an active partner in their own health, which is huge for getting them to stick to treatment plans and ultimately leads to better outcomes.
Built-in Operations and Financial Management
One of the biggest time-sucks in any practice is the disconnect between clinical work and the back office. Manually moving information from a patient chart over to the billing software is a recipe for mistakes and wasted hours. A truly modern EMR gets rid of that gap completely.
You need a system where scheduling, charting, and billing are all part of the same seamless flow. When a provider signs off on a chart, the right codes should be generated and a claim created automatically. This kind of native integration is a major dividing line when you look at different EMR systems, as it gets you paid faster and with fewer denials.
The Make-or-Break Importance of Interoperability
If there’s one feature that can make or break your entire workflow, it’s interoperability. This is just a fancy word for how well your EMR "talks" to other systems. Your practice isn't an island; you're constantly sharing information with labs, pharmacies, imaging centers, and other specialists. Without this, your staff is stuck on the phone, glued to the fax machine, or manually typing in lab results.
This isn't just inefficient—it can be downright risky. One study found that clunky systems that don't communicate well can cause serious disruptions and even lead to medical errors. When you're talking to vendors, you have to grill them on this. How, specifically, does their system connect to the labs and pharmacies you actually use? A platform built for true integration handles this from the ground up, letting data flow securely where it needs to go and creating a much safer, more connected web of care.
The Hidden Costs of a Fragmented Software Stack
Many practices don't realize how much they're bleeding resources by duct-taping a bunch of different software tools together. On the surface, juggling 8 to 12 different vendors might seem like a necessary evil, but this patchwork approach creates enormous hidden costs that have nothing to do with your monthly subscription fees. The real price is paid in lost productivity, staff burnout, and gaping security holes.
Think about it. Each piece of software has its own login, its own quirky interface, and its own support team to call when things go wrong. Your staff spends their day toggling between screens, manually copying and pasting patient information, and trying to fix integrations that constantly break. This isn't just inefficient; it’s a recipe for exhaustion.
The True Price of Disconnected Systems
When your EMR, billing software, and patient portal can't communicate, your practice feels the pain. This operational friction quietly chips away at your bottom line, day in and day out.
Just look at these common financial drains:
- Wasted Staff Hours: Every minute spent managing vendor contracts, sitting through different training sessions, or fixing data sync errors is a minute not spent with patients or on tasks that actually make money.
- Costly Errors: Manually re-keying data is the number one cause of billing mistakes, denied claims, and clinical errors. These aren't just small oopsies; they can have serious financial and compliance repercussions.
- Subscription Bloat: It's easy to end up paying for the same features across multiple platforms. You might be footing the bill for three different scheduling tools just because none of your main systems talk to each other.
The real kicker is the lack of accountability. When something breaks, every vendor points a finger at someone else, and you're the one stuck in the middle trying to solve the problem. A single partner takes that entire blame game off the table.
A Security Nightmare Waiting to Happen
Beyond the daily operational grind, a fragmented software stack is a massive security risk. Think of your practice's data security like a house. A unified system is a modern home with one strong front door and a state-of-the-art alarm. A fragmented stack is a rickety old house with a dozen different doors, each with a different lock from a different decade.
Every single piece of software is another potential way for hackers to get in. It makes doing a proper security audit a nightmare and complicates HIPAA compliance to an absurd degree. You're left hoping that every single one of your vendors has perfect security protocols, knowing that a single weak link can bring the whole thing down. For a closer look at this issue, our guide on medical practice IT support dives into why a unified security strategy is so critical.
The Value of a Single Secure Ecosystem
This is where the conversation about different EMR systems needs to go beyond just features and look at the underlying philosophy. Opting for a vertically integrated platform isn't just about making life easier; it's a fundamental business decision to streamline your operations and bulletproof your security.
With one ecosystem from a single, accountable partner, you immediately gain:
- Simplified Compliance: You manage one set of security standards and one Business Associate Agreement (BAA). That's it.
- Unified Audits: You get clear, comprehensive audit trails that show who accessed what, and when—all in one place.
- Reduced Risk: Fewer points of failure and a single expert team whose only job is to protect your data.
When you get rid of the operational drag and security risks of a disjointed tech stack, you give your team the freedom to focus on what they do best: providing outstanding care to your patients.
Frequently Asked Questions About EMR Systems
It's completely normal to have a ton of questions when you're wading through the EMR market. Getting clear answers is the only way to feel confident you're making the right call for your clinic's future. Let's tackle a few of the big questions we hear all the time from practice owners.
Which EMR Is Better if My Practice Is Growing Quickly?
For a practice on a high-growth trajectory, a cloud-based EMR is almost always the smarter bet. Think of it like this: their subscription models are built for flexibility. You can add a new provider, a new front-desk person, or even a whole new location without having to buy and install a bulky new server.
This kind of agility means your EMR grows with you, not against you. An on-premise system, on the other hand, forces you to sink a lot of money and planning into hardware every time you want to expand.
What Is the Biggest Mistake Practices Make When Switching EMRs?
Hands down, the most common and expensive mistake is overlooking the details of data migration and staff training. We're talking about years of sensitive patient data. Moving it from one system to another is a delicate operation, and if it's not done right, the integrity of your records is at risk.
A botched data transfer or a team that doesn't know how to use the new software can bring your practice to a grinding halt. You absolutely have to partner with a vendor who has a rock-solid, step-by-step migration plan and offers real, hands-on training for your entire team. It's the only way to ensure a smooth switch.
Why Can’t I Just Use a Generic EMR for My Clinic?
Trying to force a generic, one-size-fits-all EMR into a specialty practice is a recipe for daily frustration. These systems are built for primary care and just don't have the specific workflows you rely on.
A medspa needs aesthetic charting and tools to sell treatment packages. A concierge practice needs to manage membership tiers. A generic system just doesn't do that, forcing your staff into clunky workarounds that slow them down and increase the chance of mistakes. A purpose-built EMR that actually fits your clinic's flow makes everyone's job easier and improves the care you can provide.
Ready to escape the chaos of a fragmented tech stack? Ragnar STACK delivers a single, vertically integrated ecosystem purpose-built for modern practices, eliminating friction and unlocking growth. Discover the unified approach.