Technology solutions for healthcare are simply the digital tools—think electronic health records, telehealth platforms, or automated scheduling—that take the place of manual paperwork. These systems are what allow a modern medical practice to run efficiently, keep data secure, and give patients a far better experience.
Why Your Practice Runs on Technology, Not Paperwork
Let's be honest, trying to juggle a dozen different systems for booking, patient records, billing, and communication just creates headaches. It slows down your staff, it frustrates your patients, and it puts sensitive information at risk.
Running a modern medical practice on paper files and a patchwork of disconnected software is like trying to navigate a highway on a bicycle. It's not just inefficient; it's completely unsustainable.
The real challenge for private practices today, whether you're a primary care clinic or a medspa, is to cut through all that complexity. Having an integrated technology ecosystem isn't a luxury anymore—it's the basic foundation for growth and providing top-notch patient care. Think of it as your practice's central nervous system, making sure information flows exactly where it needs to, smoothly and securely.
The Problem with Disconnected Systems
When your practice is running on a hodgepodge of different software, you're essentially creating information silos. Maybe the front desk uses one system for scheduling, your clinicians use another for patient notes, and the billing department is on a totally separate platform.
This kind of fragmentation inevitably leads to the same old problems:
- Endless Data Re-entry: Your staff burns precious time just copying information from one system to another, and every time they do, it's an opportunity for a mistake.
- A Rough Patient Experience: Patients get annoyed when they have to provide the same information over and over. Appointments get mixed up, and important follow-up communication simply falls through the cracks.
- Major Security Risks: Trying to manage security and HIPAA compliance across 8-12 different vendors is a nightmare. Each one is another potential weak point for a data breach.
- Operational Drag: Simple, everyday tasks become needlessly complicated. This slows down everything from the moment a patient walks in the door to getting paid for your services.
The point of healthcare technology isn't just to get rid of paper. It's to eliminate the operational friction that gets in the way of focusing on what really matters: your patients. An effective solution pulls every part of your practice into a single, cohesive unit.
Building a Foundation for Growth
Consider this guide your playbook for turning that technological chaos into a genuine competitive advantage. We're going to walk through the key categories of technology solutions for healthcare that solve these daily frustrations, from the core software to more advanced automation tools.
For a deeper dive into the administrative backbone that holds a clinic together, you can learn more about what practice management software is and how it works.
By the time you're done, you'll have a clear, practical roadmap for figuring out what you need, choosing the right tools, and building a practice that's efficient, secure, and ready for whatever comes next. It’s time to move past the paperwork and build a practice that runs on a smart, integrated technology stack.
What's in Your Core Technology Toolkit?
Building a modern, efficient practice isn't about just having good intentions; it's about having the right digital tools working together. Think of your practice's technology as a specialized toolkit. Each instrument has a very specific job, but they’re all designed to fit together perfectly. When they don't, you get chaos.
Diving into the world of healthcare technology solutions can feel like a lot to take on, but it really just comes down to a few core components that solve the real, everyday problems your practice faces. Let's break down the essential pieces of this puzzle, cutting through the jargon to see what they actually do for your team and your patients.
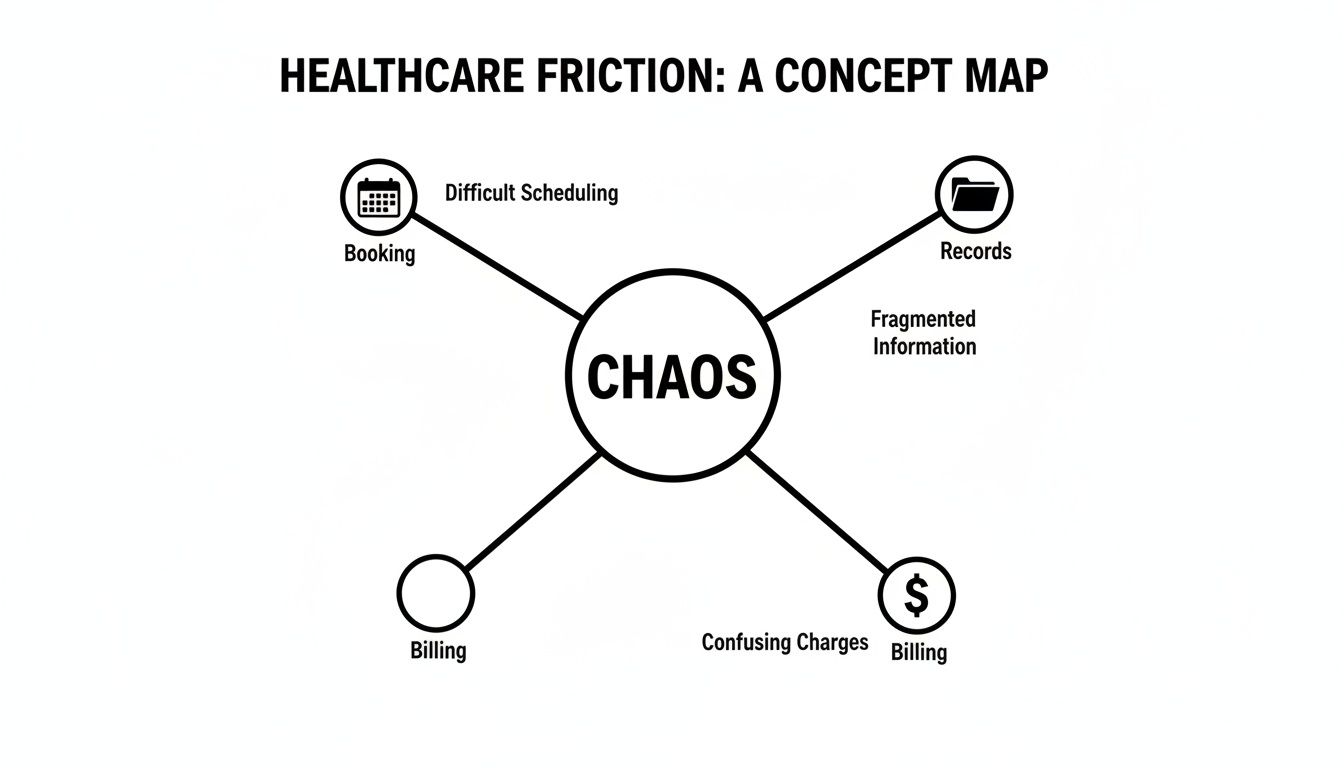
The image below shows the biggest friction points in a typical practice—exactly where technology can make the biggest difference.
As you can see, when booking, records, and billing are all disconnected, you end up with operational headaches. A unified tech toolkit is built to solve exactly that problem.
To give you a clearer picture, here’s a quick overview of the essential technology categories every modern practice should consider.
Key Technology Solutions for Modern Practices
| Technology Category | Core Function | Benefit to Practice | Benefit to Patient |
|---|---|---|---|
| Electronic Health Records (EHR) | Manages all clinical patient data in a single, secure digital record. | Faster decision-making, reduced errors, and improved care coordination. | Safer care, a complete health history, and better treatment outcomes. |
| Practice Management Software (PMS) | Automates administrative and business tasks like scheduling and billing. | Increased staff efficiency, faster revenue cycle, and smoother operations. | Easier appointment booking and more accurate, transparent billing. |
| Patient Engagement & Telehealth | Facilitates communication and virtual care between visits. | Fewer no-shows, better patient relationships, and increased accessibility. | Convenient access to care, appointment reminders, and a stronger connection. |
| Cybersecurity & Compliance | Protects sensitive patient data from breaches and ensures HIPAA adherence. | Mitigated risk, protected reputation, and avoidance of costly fines. | Confidence that their personal health information is safe and secure. |
| Integrations & Interoperability | Connects disparate systems to allow for seamless data sharing. | A single source of truth, eliminates data silos, and automates workflows. | A frictionless experience where their data follows them seamlessly. |
Each of these pieces plays a critical role. Let's dig a little deeper into what each one does.
Electronic Health Records: The Digital Patient Story
At the very heart of any modern practice is the Electronic Health Record (EHR) system. It's time to say goodbye to bulky paper charts and misplaced files. An EHR is the single, secure, digital narrative of a patient's entire health journey.
Think of it as a patient's living biography. It holds their medical history, diagnoses, medications, treatment plans, immunization dates, allergies, and lab results. For your clinicians, this means having a complete picture at their fingertips, leading to better, faster, and safer decisions.
An EHR is so much more than a digital filing cabinet. It's an active clinical partner that serves up critical information right at the point of care, dramatically cutting down the risk of errors and improving patient outcomes.
Instead of a staff member spending precious minutes hunting for a physical chart, a physician can pull up a patient's full history in seconds. This kind of immediate access isn't just a nice-to-have during a routine appointment; it's absolutely essential in an emergency. A well-implemented EHR is the foundation on which everything else is built.
Practice Management Software: The Operational Command Center
While the EHR manages the clinical side of things, Practice Management Software (PMS) handles the business side. If the EHR is the patient's story, the PMS is your clinic's operational command center. It’s the engine that keeps your practice running day in and day out.
This software automates and simplifies the administrative tasks that eat up so much of your staff's time. Its core functions are designed to make operations flow smoothly from the front desk to the back office.
- Appointment Scheduling: It manages the entire booking process, from letting patients schedule themselves online to handling complex calendars for multiple providers.
- Medical Billing and Coding: The software automates the creation of claims, scrubs them for errors before they're submitted, and tracks payments, which significantly speeds up your revenue cycle.
- Patient Registration and Demographics: It captures and stores all the necessary patient information, which means less manual data entry and fewer mistakes.
A good PMS gets rid of countless manual tasks, freeing up your team to focus on what really matters: interacting with patients. You can get a more detailed look at the power of healthcare practice management software and how these systems drive real efficiency.
Patient Engagement and Telehealth Platforms
Today, healthcare happens well beyond the four walls of your clinic. Patient engagement platforms are the tools that help you build and maintain strong relationships with your patients between visits. They usually include things like secure patient portals, automated appointment reminders, and tools for sending out educational materials.
Telehealth platforms take this a step further, acting as the modern-day "virtual house call." These secure video conferencing tools break down geographical barriers, making care more accessible and incredibly convenient for your patients. Their value became undeniable in recent years, and they are now a standard part of care delivery for practices of all sizes and specialties. Put together, these tools create a much better and more connected patient experience.
How AI and Automation Are Changing Clinical Workflows for the Better
Artificial intelligence isn't some far-off concept from a sci-fi movie anymore. It's a real, practical tool that's already making a huge difference in clinical efficiency. Many of the best technology solutions for healthcare now have AI built right in, specifically to tackle the mountain of administrative work that bogs down a clinician's day. It's all about giving precious hours back to your doctors and staff.
This isn't just about speed; it's about focus. When a physician can give their full attention to the person in front of them instead of a computer screen, everyone wins. That’s the real-world promise of AI in a clinical setting.
And practices are catching on fast. The global AI in healthcare market has already hit $36.96 billion and is expected to explode to $613.81 billion by 2034. While only 38% of U.S. physicians were using AI a few years back, that number has shot up to 66%. Think about this: it took 15 years for EHRs to become standard, but tools like ambient AI scribes got there in just 2-3 years. You can learn more about these dramatic shifts in healthcare AI adoption and what they mean for the industry.
AI Scribes and Automated Documentation
One of the most powerful and immediate uses of AI is the ambient AI scribe. Just picture an intelligent assistant in the exam room that listens to the conversation between a doctor and patient, then automatically creates a structured, accurate clinical note right inside the EHR.
This one piece of technology directly attacks physician burnout at its source: documentation. Instead of spending hours after work typing up notes, clinicians can finally be fully present during the consultation, building the trust and rapport that’s so essential to good care.
The impact is immediate and obvious:
- A Lighter Administrative Load: Doctors get several hours back each week. That’s more time for patients, for professional development, or even just for a healthier work-life balance.
- Better, More Accurate Notes: AI scribes capture the nuances of a conversation that might get lost in manual note-taking, resulting in a more complete and precise patient record.
- A Stronger Doctor-Patient Connection: When a doctor can maintain eye contact and have a natural conversation, the patient feels seen and heard, which dramatically improves their overall experience.
Predictive Analytics for Getting Ahead of Health Problems
Beyond just cleaning up documentation, AI is also becoming an incredible tool for proactive patient care. Predictive analytics uses smart algorithms to comb through years of patient data in your EHR, spotting patterns that can help predict future health risks.
Think of it like having an incredibly advanced weather forecast for your patient's health. Instead of waiting for a health crisis to strike, you can see the storm clouds gathering and take action before things get serious.
Predictive analytics fundamentally changes the care model from reactive to proactive. It gives providers the foresight to step in early, manage chronic conditions more effectively, and stop preventable hospital visits before they ever happen.
For instance, an algorithm could flag a patient with diabetes who, based on recent lab work, medication history, and lifestyle factors, is at a high risk for a heart attack. This gives the care team a heads-up to reach out with targeted support, like a medication adjustment or a priority follow-up appointment.
Putting Repetitive Clinical Tasks on Autopilot
So many clinical workflows are bogged down by repetitive, manual tasks that eat up staff time but don't require any clinical judgment. This is where simple automation becomes a game-changer, making sure important steps are never missed.
Take patient follow-up, for example. Automation can handle the routine parts of this process flawlessly, ensuring every patient gets the same high level of attention.
- Automated Appointment Reminders: The system sends out texts or emails to patients, which is proven to slash no-show rates.
- Post-Visit Follow-Up: After a visit, patients can automatically receive care instructions, educational materials, or a link to a satisfaction survey.
- Lab Result Notifications: Patients get a secure message through their portal the moment their lab results are in, with clear instructions on what to do next.
By letting technology handle these routine jobs, you free up your nurses and medical assistants to focus on the human side of healthcare—things like patient education and coordinating complex care. These small efficiencies really add up, leading to a much smoother, more effective, and more responsive practice.
The Power of a Unified Technology Ecosystem
Trying to run a modern medical practice with a dozen different software vendors is like trying to conduct an orchestra where every musician is playing from a different sheet of music. It's chaotic, inefficient, and the final result is never what you hoped for. This problem, what we call "vendor sprawl," creates a tangled web of hidden costs that quietly sap your practice's energy and resources.
When every piece of your tech stack—from the EHR to the billing portal—operates in its own silo, you're constantly battling integration failures, security gaps, and the sheer frustration of juggling multiple support lines. Each separate system is another potential point of failure just waiting to happen.
This is why so many savvy practices are moving away from this patchwork approach and embracing a unified platform. Imagine a single, cohesive system where patient information flows seamlessly from an online appointment request to the clinical chart and straight through to billing, all without a single copy-paste.
The Hidden Costs of Vendor Sprawl
Sure, the most obvious cost of using multiple vendors is the stack of subscription invoices you pay each month. But the real damage comes from the operational friction this fragmented setup creates. These indirect costs are often far more significant.
- Wasted Staff Hours: Think about how much time your team loses just logging in and out of different systems or manually re-entering patient data. That's time they could be spending with patients, but instead, it's lost to administrative busywork.
- Increased Error Rates: Every time someone has to manually transfer information, the risk of a mistake goes up. A typo can lead to a denied claim, a billing headache, or worse, a clinical safety issue.
- Compliance Nightmares: Keeping one system HIPAA compliant is a big enough job. Now imagine trying to manage that across 8-12 different vendors, all with their own security policies and update schedules. It's a recipe for a compliance disaster.
This disjointed approach doesn't just hurt your bottom line; it grinds down your team. The constant workarounds and technical glitches are a direct path to staff burnout and frustration.
Advantages of a Single Integrated Platform
Switching to a unified ecosystem isn't just about convenience—it's a smart strategic move. You're trading complexity for clarity, allowing your practice to run with far more precision and security. The benefits show up almost immediately and build a solid foundation for growth.
With a single platform, you have one partner to call for all your tech needs. No more guessing which vendor is responsible when something breaks. You have one team that understands your entire workflow, which simplifies troubleshooting and creates clear accountability. To learn more about how a dedicated partner can streamline operations, check out our guide on medical practice IT support.
By consolidating technology into a single, cohesive ecosystem, you transform your practice's IT from a collection of disjointed tools into a strategic asset. This single source of truth eliminates data silos and provides a complete, 360-degree view of both patient health and practice operations.
This consolidation brings powerful, real-world advantages you'll notice every single day.
- Seamless Data Flow: Information gets entered once—at the front desk or by the patient online—and is instantly available to clinicians in the exam room and the billing team in the back office. No more redundant data entry.
- Centralized Security: All your sensitive data is protected under one robust security umbrella. This makes it infinitely easier to manage user access, monitor for threats, and maintain a consistent, HIPAA-compliant environment.
- Improved Patient Experience: From the patient's point of view, everything just works. They can schedule appointments, complete forms, and message your staff through one easy-to-use portal, giving your practice a professional, modern feel.
At the end of the day, your technology should make your job easier, not harder. A unified ecosystem provides the reliable backbone that frees your team to focus on what truly matters: providing outstanding patient care. This holds true whether you’re running a busy primary care clinic, a high-end medspa, or a personalized concierge practice.
Getting New Technology Right the First Time
Bringing new technology into your practice isn't just about buying the latest software. It's about a smart, people-first strategy. A rushed rollout almost always creates more problems than it solves, leaving you with frustrated staff, broken workflows, and a terrible return on your investment. The only way to get this right is with a deliberate, thoughtful approach.
The real work starts long before you ever sign a contract. It begins with a hard look at your practice's current state—what are the real bottlenecks? Where are the genuine pain points you need to solve? This isn't just an IT project; it's a clinical and operational one that needs input from everyone who will actually use the new tools.
Start with a Workflow Assessment
Before you can fix your processes, you have to understand them inside and out. A workflow assessment is a deep dive into how your practice actually operates day-to-day. Think of it as drawing a detailed map of how work gets done, from patient check-in to final billing.
This step is critical for spotting the hidden inefficiencies. Maybe your front desk team spends an hour every afternoon manually matching appointment data between two different systems. Or perhaps your clinicians are slowed down by an EHR that takes ten clicks to do something that should take two.
A proper assessment brings these friction points to light. It gives you a clear set of goals for any new technology, ensuring you pick a solution that solves the problems you actually have.
Get Your Team Involved from Day One
The number one reason new technology fails? A lack of team buy-in. If your staff feels like a new system is being forced on them, they’ll find a thousand reasons why it won't work. The best way to get them on board is to include them from the very beginning.
Pull together a small selection committee with people from different roles:
- Clinicians: They can speak to a system’s usability where it matters most—in the exam room.
- Front Desk Staff: They know exactly what makes a scheduling and registration tool a lifesaver versus a headache.
- Billing Specialists: They can put the revenue cycle management features through their paces.
When your team has a real sense of ownership in the decision, they become champions for the new system. That's absolutely essential for a smooth launch and long-term success.
Plan for a Smooth Switch
Once you've found a true technology partner—not just another vendor—the real work of implementation begins. A good partner will walk you through a structured plan that puts continuity of care above all else.
A successful technology transition should feel like a carefully planned upgrade, not a chaotic overhaul. The goal is to enhance what you do without ever disrupting the patient experience or overwhelming your team.
Here’s what that process should include:
- Data Migration: Your partner must have a proven, secure process for moving all of your patient data from the old system to the new one, accurately and without any gaps.
- Hands-On Staff Training: Training needs to be specific to each person's role. Every single team member should feel confident using the new tools before you go live.
- Measuring Return on Investment (ROI): You need to define what success looks like ahead of time. Is it reducing patient wait times? Speeding up the billing cycle? Cutting down on staff overtime? Whatever it is, you need a clear way to measure the impact.
Thankfully, the trend toward integrated, cloud-based platforms is making this whole process simpler. With cloud adoption in healthcare now past 80%, practices are finding it easier to manage data and stay updated. By bringing systems together, clinics can often shrink their vendor list from as many as 8-12 down to a single partner, which means smoother data flow and simpler compliance. For a deeper look at these market shifts, you can discover more insights about healthcare technology trends on svitla.com.
Choosing the right platform can make all the difference, and our guide on the best practice management software is a great place to start weighing your options.
Building Your Tech-Enabled Practice
So, let's pull all these threads together. The point of all this technology isn't to replace the human touch in medicine. It’s to get rid of the operational headaches so you and your team can focus on what actually matters: your patients.
When your systems are all speaking the same language, the benefits are real and immediate. You get a more efficient clinic, stronger security, and a patient experience that actually feels modern and supportive. The next move is yours: take an honest look at your current tools, find the biggest sources of daily frustration, and see how a unified technology solution for healthcare can fix them.
From Assessment to Action
Don't think of this as a massive IT project. It's really just a strategic look at how your practice runs. You start by pinpointing where things are breaking down—is it staff time wasted on manual tasks? Is it a clunky patient intake process causing no-shows? Maybe it's billing errors that are quietly costing you a fortune.
A good technology partner won’t just sell you software; they’ll walk you through this evaluation.
The whole idea is to build a tech stack that fits your practice like a glove, whether you're a bustling primary care office, a high-end specialty medspa, or a concierge clinic. It's about finding those specific opportunities to make workflows smoother for everyone who has to use them.
Ultimately, you’re trying to build a practice that’s not just more profitable and secure, but one that’s a genuinely better place for your team to work and for your patients to receive care. That’s how you create an advantage that lasts.
Your Path Forward
Moving toward an integrated tech strategy is your chance to build a stronger, more patient-centric practice. It’s the difference between juggling a dozen different vendors and having one accountable partner who understands your big-picture goals.
Ready to start? Here’s a simple game plan:
- Map your workflows: Get a clear picture of how things get done day-to-day and find the bottlenecks. Where do things get stuck?
- Talk to your team: They're on the front lines. Ask them what their biggest daily frustrations are with the current systems.
- Set clear goals: What do you actually want the technology to do for you? Do you want to reduce no-shows by 20%? Cut down on billing paperwork by 10 hours a week?
Taking these steps ensures you choose a solution that doesn't just solve today's problems but grows with you. It’s time to build a practice that runs on a smart, connected foundation—one designed for what healthcare will look like tomorrow.
Frequently Asked Questions
When it comes to bringing new technology into a practice, clinic owners and managers always have questions. It's a big decision. Here are some straightforward answers to the most common concerns we hear.
Are These Advanced Systems Really Affordable for a Small Practice?
Yes, they absolutely can be. The best modern platforms are built to scale, so they're not just for huge hospital systems. For a smaller practice, the key is to stop thinking about it as just an upfront cost and start looking at the return on investment (ROI). A truly integrated system gives you back countless staff hours, cuts down on costly human errors, and helps you keep patients coming back.
Think about it this way: many practices are juggling anywhere from 8-12 separate software vendors. By bringing all that under one roof with a single technology partner, you're not just getting rid of a dozen different subscription fees. You're also cutting out the hidden costs and headaches of trying to make all those disconnected systems talk to each other. A good partner will sit down with you and map out exactly where you'll see the biggest wins, both financially and in your day-to-day operations, proving the solution will pay for itself.
How Do We Switch to a New System Without It Being a Total Nightmare for Our Patients?
A chaotic transition is a completely avoidable problem. It all comes down to planning and working with a partner who knows what they're doing. The secret is finding a provider who gives you a dedicated implementation team to walk you through the entire process, from start to finish.
That process has to cover a few critical things:
- A rock-solid plan for migrating your data securely and accurately.
- Real, hands-on training for your team that’s specific to their jobs.
- A gradual, phased rollout so you're not trying to change everything at once.
You don't just flip a switch and go live with a new system. A successful transition always begins with a deep dive into your current workflows. The goal is to set up the new system to make those processes better from day one, so the change feels like a natural improvement for your staff and your patients.
With the right people guiding you, the switch can happen in the background without ever disrupting the rhythm of patient care.
What's the Single Biggest Security Risk We Face with Technology Today?
Honestly, the biggest risk isn't some super-sophisticated hacker. It's a fragmented tech setup. When you rely on a patchwork of different vendors for your EHR, scheduling, billing, and patient messaging, you’re creating a security minefield.
Every one of those separate tools has its own security rules, its own update schedule, and its own potential weaknesses. Trying to keep everything secure and HIPAA-compliant is a nightmare. It’s like trying to guard a house where every window and door has a different lock from a different company—it's just a matter of time before one fails.
The most powerful way to lock things down is to move to a unified, single-vendor platform. This centralizes all your security management, makes compliance simpler, and ensures every part of your system was designed to work together securely from the ground up. You get one, clean audit trail, which drastically lowers your practice's risk profile.
At Ragnar STACK, we get rid of the complexity and risk that comes from juggling multiple vendors. Our vertically integrated technology ecosystem was built from the ground up to harden security, simplify workflows, and deliver an incredible patient experience. See how our single-partner approach can change your practice by exploring our platform at https://notes.rstack.io.